If new information becomes available, progress (or the lack thereof) occurs, additional problems arise, or the simple passage of time means a treatment plan update is needed, note that too, as a prompt to do the update next session. Other guidelines for DAP notes. Does the note connect to the client’s individualized treatment plan? Are client strengths/limitations in achieving goals noted and considered? Is the note dated, signed and legible? Is the client name and/or identifier included on each page? Has referral and collateral information been documented?
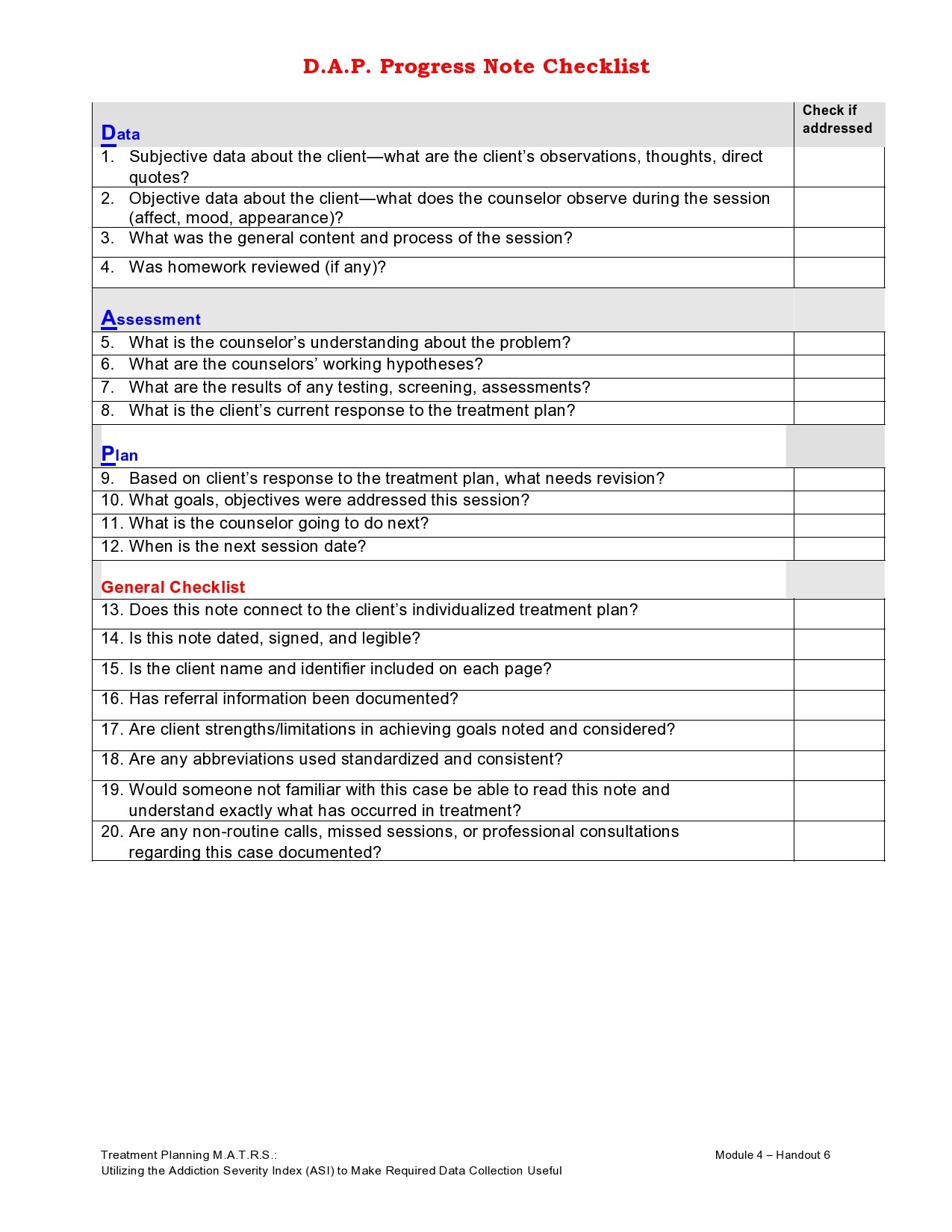
Data, Assessment, Plan. These are the fundamental building blocks of the DAP note. While they serve the same purpose as a SOAP note, DAP is a slightly different format. What you choose is entirely up to personal preference. This article should help you understand the basics of DAP notes and how to use them in your behavioral health practice.
What is a DAP note?

A DAP note is a method of documentation used by health care providers, social workers and similar professionals. While SOAP is a more popular format in medicine, the Data, Assessment, Plan paradigm is potentially more appropriate for behavioral health.
The Basics of DAP
- Data — this section includes observable and identifiable behaviors and traits. This section answers the question “What did I see during the session?”
- Assessment — this is about the meaning of the data. This includes clinical findings. Essentially, it answers the question, “What does the data mean?”
- Plan — this wouldn’t be a complete treatment plan, that would be on another document. (See our other article Writing Great Mental Health Treatment Plans for more detail on treatment plans.) The Plan section in a DAP note is where you answer the question, “What will I do in light of the Assessment.”
Some practitioners add “Response” to the Assessment section (i.e. DARP note,) however, this is really just an extension of the assessment. This would be where you would record the client’s response to the assessment. It’s a helpful mental tool for you to expand on the Assessment section; use it if you want. In mental health treatment especially, the client’s response can be valuable information as their response determines the effectiveness of any plan you might make.
SOAP or DAP? Which is better for mental health?
SOAP has traditionally been the “industry standard” for clinical notes. This is a result of the influence of the medical profession. While behavioral health, specifically non-psychiatric behavioral health treatment, is “health care,” counseling and therapy doesn’t have the benefit of the same sorts of diagnostic data as does medicine.
If new information becomes available, progress (or the lack thereof) occurs, additional problems arise, or the simple passage of time means a treatment plan update is needed, note that too, as a prompt to do the update next session. Other guidelines for DAP notes. Does the note connect to the client’s individualized treatment plan? Are client strengths/limitations in achieving goals noted and considered? Is the note dated, signed and legible? Is the client name and/or identifier included on each page? Has referral and collateral information been documented?
Data, Assessment, Plan. These are the fundamental building blocks of the DAP note. While they serve the same purpose as a SOAP note, DAP is a slightly different format. What you choose is entirely up to personal preference. This article should help you understand the basics of DAP notes and how to use them in your behavioral health practice.
What is a DAP note?
A DAP note is a method of documentation used by health care providers, social workers and similar professionals. While SOAP is a more popular format in medicine, the Data, Assessment, Plan paradigm is potentially more appropriate for behavioral health.
The Basics of DAP
- Data — this section includes observable and identifiable behaviors and traits. This section answers the question “What did I see during the session?”
- Assessment — this is about the meaning of the data. This includes clinical findings. Essentially, it answers the question, “What does the data mean?”
- Plan — this wouldn’t be a complete treatment plan, that would be on another document. (See our other article Writing Great Mental Health Treatment Plans for more detail on treatment plans.) The Plan section in a DAP note is where you answer the question, “What will I do in light of the Assessment.”
Some practitioners add “Response” to the Assessment section (i.e. DARP note,) however, this is really just an extension of the assessment. This would be where you would record the client’s response to the assessment. It’s a helpful mental tool for you to expand on the Assessment section; use it if you want. In mental health treatment especially, the client’s response can be valuable information as their response determines the effectiveness of any plan you might make.
SOAP or DAP? Which is better for mental health?
SOAP has traditionally been the “industry standard” for clinical notes. This is a result of the influence of the medical profession. While behavioral health, specifically non-psychiatric behavioral health treatment, is “health care,” counseling and therapy doesn’t have the benefit of the same sorts of diagnostic data as does medicine.
In a SOAP note, the Subjective section is where you record subjective feelings (obviously enough.) The problem with behavioral health is that much of your session is inherently subjective. Meaning, it’s difficult to take the “temperature” of a therapy client — a temperature is an indisputable fact, while, “appears to be falling asleep,” could be considered subjective.
Pediatric Darp Notes Examples
Essentially, the problem with the Objective section is that many of the things you are recording aren’t quantifiable. Can you measure the degree of which a patient “appears to be falling asleep?” Can you compare that to another patient who is also “appearing to fall asleep?” It’s pretty hard and, unless you’re measuring vital signs and perhaps brainwaves during a session, ultimately, that observation is mostly subjective, however in a behavioral health SOAP note, that “appears to be falling asleep,” would be assigned to the Objective section. It can get confusing simply because of the nature of a therapy session. It’s great for medicine as “The patient has a 99.3 temperature” is clearly objective, but it can get murky when you’re dealing with mental health.
What Is A Darp Note
The Subjective and Objective sections of your note often begin to merge together in a behavioral health context. However, with a DAP note, that merging isn’t problematic, since it would all be recorded under the Data section.
Pediatric Darp Notes Examples
It’s really just a mental exercise in terminology and how you record information, but in my opinion, DAP is a superior choice simply because it eliminates any ambiguity and gives you a clearer mental model with which to organize your thoughts.
Nursing Darp Notes
DAP or SOAP — whatever you use is entirely up to you (or your administrators,) the important thing is to be consistent, record the data, and stay methodical and organized.
What clinical note formats do you use in your practice? Have any tips you’d like to share with the community? Leave a comment below and let us know!
